For most long-term care and skilled nursing operators, pharmacy costs are the largest expense outside labor making management exceptionally critical in order to deliver medication to patient populations successfully and control costs.
Selecting the right pharmacy partner and ensuring the efficacy of a pharmacy contract can have significant and long-lasting effects for operators.
While some LTC operators may be limited in selecting pharmacy partners due to geographic constraints, most operators have options when selecting a partner. Like with most vendors, partner selection should depend on multiple factors including price, contract terms, reputation, offerings, and customer service. The complexity of the billing process also demands that operators can establish a relationship based on trust, transparency, and accountability.
Melissa Beckstead, Director of Pharmacy Operations at SRX, works closely with LTC operators to integrate technology into their pharmacy spend management in order to reduce pharmacy costs. “We frequently work with operators to establish better solutions around their pharmacy spend—that obviously involves looking closely at their pharmacy contracts. What we see is a wide range of contract terms, pricing models, data and reporting delivery methods, and level of service. Good pharmacy partners work with facilities to make a positive impact on this critical cost center for operators.”
The following are three key areas that LTC and skilled nursing operators should look at when evaluating a pharmacy partner or re-evaluating a pharmacy contract.
Transparent Pricing Terms
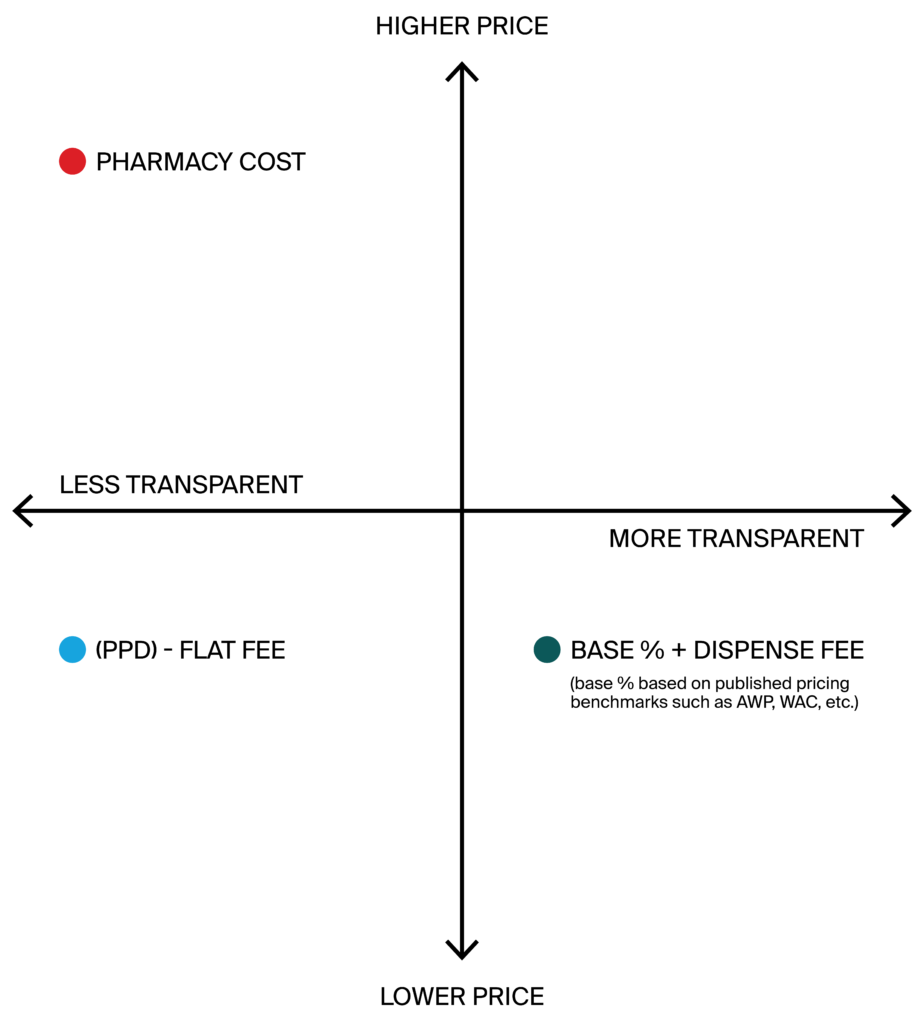
Do you know how much you are paying your pharmacy partner? You might understand that large figure at the bottom of your bill each month, but it might be hard to tell if what you are paying matches what you agreed to pay. Pricing terms vary from pharmacy to pharmacy and understanding your cost and pricing structure is essential to understanding your pharmacy spend.
Best Practices
A good pharmacy partner and contract should represent fair and transparent pricing for both parties. This means that pricing is based on published drug pricing sources that include one of the following:
- Average wholesale pricing (AWP)
- Wholesale acquisition cost (WAC)
- National Average Drug Acquisition Cost (NADAC)
- ACA Federal Upper Limits (FUL)
Typically, pricing models that use published pricing adhere to a base + dispensing fee. This structure allows operators to verify pricing and know exactly how their costs are calculated.
Beckstead and her team also help LTC operators evaluate pharmacy contracts and control costs. In her experience, most operators don’t fully understand their pharmacy contract terms. “Many of our customers are in contracts that are confusing and structured to benefit the pharmacy, not facilities. When we partner with customers, we are able to help them evaluate their contracts against others when it’s time for renewal. We have sophisticated technology and experts that help operators know what to look for which helps them to negotiate much more favorable terms with a new pharmacy. They know exactly what they are paying for which puts them in control and saves both time and money.”
Poor Practices
Suppose a pharmacy is billing operators and facilities at “pharmacy cost” as opposed to published pricing as outlined above. In that case, there is no way to verify what the pricing should be based on the actual cost to the pharmacy. Additionally, flat-fee arrangements don’t protect either the pharmacy or the operator from drug price fluctuations on the market. Often, flat-fee arrangements require reconciliation at a later point in time, which can be cumbersome, time intensive, and costly for both parties.
Rebate Payments
Drug manufacturer rebates represent a significant opportunity for operators to recoup pharmacy costs. As the payer for medication costs, operators should receive the rebates for eligible medications and payments that can add up to tens of thousands, if not millions, of dollars annually depending on the size of the operator. In combination with strategic drug utilization selection, operators can shift facility formularies to incorporate drug equivalents in order to maximize rebate dollars. However, this requires cooperation from pharmacies in terms of billing accuracy and transparent contract terms and conditions.
AJ Farhoud, RPh, is the pharmacy resource and consultant for Bandera Healthcare, a division of publicly-traded skilled-nursing giant The Ensign Group. In his role he is charged with overseeing the proper management of pharmacy services, both clinical and financial. As he explains, even with the right processes and partners in place, ensuring proper credit for rebates and control of what ends up on their bills is a challenge. “We used to process claims manually. It wasn’t working, especially in hindsight through the lens of having the right technology in place and improving our contracts. With those changes, the level of insight into what was actually going on was astonishing. Our rebates increased, and our costs went down. That said, we continue to run into issues where rebates aren’t processed correctly or by the right party. Just knowing those rebates belong to our facilities—which is now reflected in our contracts—has empowered us to ensure that ultimately those rebates are credited back to us.”
Best Practices
Rebate administration is often handled either by facility administrators or third party pharmacy benefits managers (PBMs) that work with pharmacy partners to submit eligible rebates. Regardless of who is handling the rebate administration, pharmacies need to provide transparent reporting for rebate eligible orders, and should clearly state within contracts that they are not submitting rebates that should belong to operators. If operators are working with PBMs or other third parties, facilities should know exactly what the PBM is receiving for administration, the amount of their total eligible rebates, what they can expect to receive, and when rebate dollars will be delivered. This requires accurate and transparent billing, reporting, and submission processes.
Poor Practices
There are pharmacies that submit and collect rebates on behalf of the operators with whom they partner. As the pharmacy is not the payer, they are not the party legally eligible for the rebates on claims submitted by LTC facilities. This may be done without the payer’s (operator) knowledge or through limited transparency in language that is vague or buried in the pharmacy contract. One indication that a pharmacy is submitting rebates for payment is if the facility receives a duplicate notification on a claim. If a contract mentions the pharmacy obtaining “drug discounts” from manufacturers, this is another indication that the contract signs away the facility’s eligibility to submit those claims.
Automated Processes
Pharmacy bills are complex. Auditing bills with hundreds of line items is not only cumbersome and inefficient, it also creates many opportunities for unidentified errors. Like any other vendor, pharmacies should be utilizing technology and automation when possible to provide accurate and timely reporting and quickly respond to audit requests and questions.
Best Practices
From pricing data to electronic health records (EHRs), to claims data and everything else that goes into a pharmacy bill, good pharmacy partners should be using available technology and processes that streamline billing, reporting, and audits. The best pharmacy partners will facilitate adjudication, which allows automation to enforce formulary and pharmacy contract rules. This prevents errors from occurring, reduces the need for chasing down credits and returns, and provides operators with the insight needed to control pharmacy spend. Adjudication can control for quantity restrictions, day supply, refills-too-soon, preferred/excluded drugs, etc. If a pharmacy isn’t using adjudication, operators should expect digital files and reports that can be exported and delivered in a timely manner.
“Adjudication can be one of the most effective tools for operators in taking more control of their pharmacy spend. Done correctly, it shouldn’t cost operators anything and allows bills to more accurately reflect actual pricing and prevent errors from occurring in the first place,” says Beckstead.
Automation and digital reporting / auditing also allow pharmacies to respond more quickly to audits and requests for information, often in real time. Good pharmacy partners will respond within 30 days to an audit request and should be responding to any other communications within 24-48 hours.
Poor Practices
Using outdated systems and technology, or even manual processes in some cases can really impact the efficiency and cost of pharmacy services. Pharmacies that send data in unusable formats limit the ability of their LTC operator partners to have complete insight into their claims, payments, and eligible rebates. Additionally, operators should expect a high level of customer service and responsiveness. Delaying responses to requests beyond 45 days should be a warning sign for operators that they may need to demand a higher level of service and support than they are receiving.
Tips for Selecting a Good Pharmacy Partner
First and foremost, operators should remember that they are the customer. Don’t be shy in requesting improvements in your pharmacy relationship or comparing alternatives if you aren’t satisfied with your contract or service. The following are some additional tips to consider when looking at partners or evaluating contracts:
- Compare Alternatives—While geography may impact the number of available pharmacy partners, most operators should have access to multiple options. Even if LTC facilities already have an established pharmacy relationship, evaluating alternatives at each contract renewal period will allow operators to make informed decisions and leverage the best pricing, terms, and services to make a final selection.
- Educate Yourself—Looking at best practices such as those outlined above will provide a basis for understanding and help identify potential red flags and areas for improvement and negotiation. ‘
- Be Specific and Request Details—Ask for sample reports, data exports, communications, etc. and demonstrations of process and procedures. This will help to set expectations and present opportunities to discuss questions and potentially request customizations that will make for a smooth relationship.
Technology & Expertise
Ultimately, taking full control of pharmacy spend and your pharmacy relationship requires integrating technology with knowledgeable expertise. SRX full technology suite provides LTC operators with the tools needed to analyze and audit bills, and control what ends up on them. One of SRX’s products reviews pharmacy contracts for operators, identifies areas of concern, and estimates potential savings that can be realized through automation, adjudication, and drug utilization. Beckstead continues, “If operators need guidance or tools to lower their pharmacy spend, SRX offers these. We work alongside our customers as partners in their pharmacy practice and relationships to ensure transparency, accountability and lowest net cost. Our services bridge a gap in this complex operational area, and our customers are better positioned to succeed.”
Want to learn more?
Related Articles:
Drug Spend Cost Savings + Rebates for Multi-Regional Operator
Dollars You Put Back into Your Long-Term Care (LTC) Facility
SRX’s Partnership Approach to Helping Long-Term Care Operators Succeed
SRX Rebates
SRX is a technology and advisory company that helps LTC operators realize the lowest net cost on pharmacy spend. We help our customers improve drug utilization, manage pharmacy relationships, reduce costs and waste, and maximize rebates. We are committed to transparency and accountability and guarantee our quarterly rebates are paid on time, every time. Contact us at 833 633 6833.
Learn more about our rebate services.